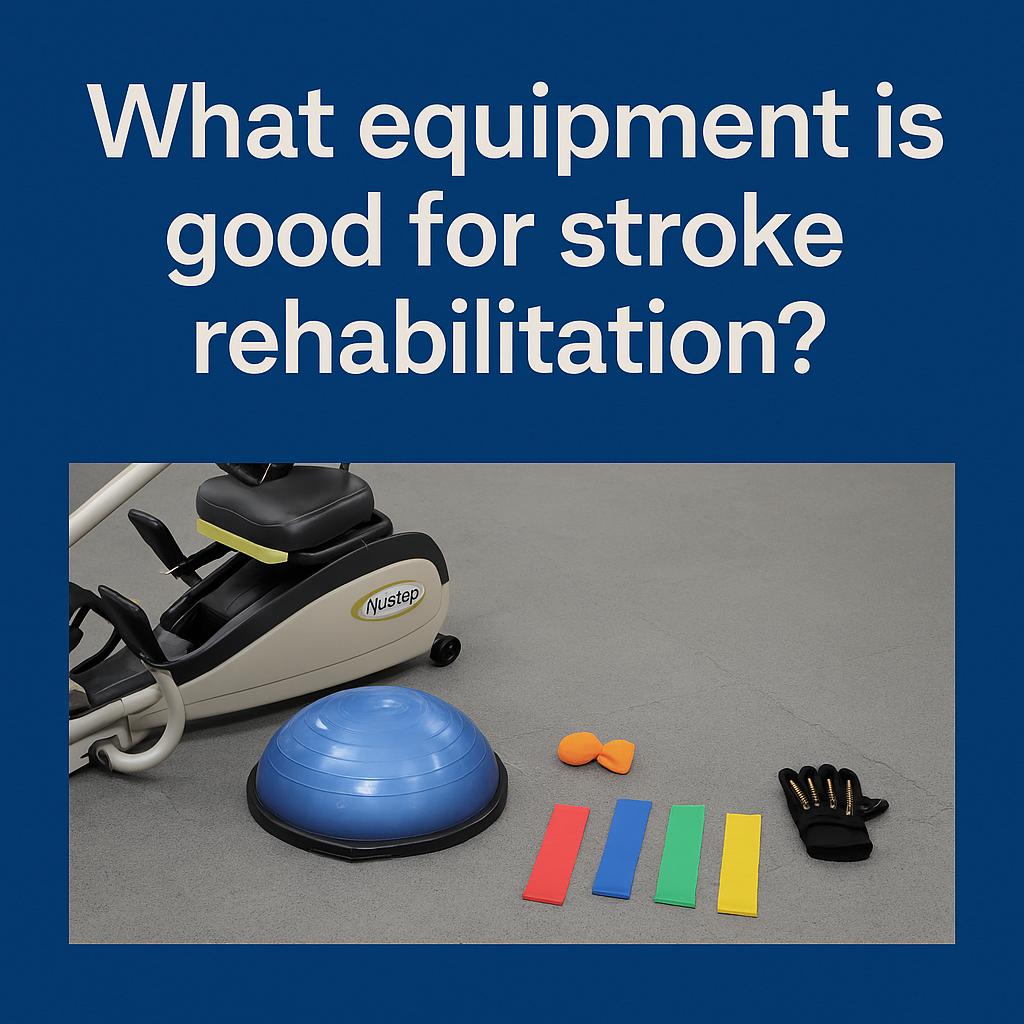
Effective stroke rehabilitation equipment includes recumbent steppers, resistance bands, and arm bikes to rebuild strength and endurance; balance tools like BOSU balls and parallel bars to improve stability; and hand therapy devices such as putty, grip trainers, and robotic gloves to restore fine motor control. For walking recovery, bodyweight-supported treadmills and FES devices retrain gait patterns and activate weakened muscles. Smart rehab robotics, pedal exercisers, and multi-functional therapy stations provide guided, repetitive motion that supports neuroplasticity. These tools work together to improve mobility, coordination, and independence during stroke recovery.
What upper limb rehabilitation tools help stroke survivors regain mobility?
Stroke survivors often experience muscle weakness or loss of movement in the upper body, particularly on one side. Regaining arm and shoulder mobility requires repetitive, targeted movement supported by specialized rehabilitation tools.
- Arm Ergometers (Arm Bikes)
These machines allow patients to pedal with their arms, improving cardiovascular endurance and joint mobility. They are particularly effective for those with limited leg function and can be adjusted for passive or active motion depending on the user’s strength level. - Therapy Resistance Bands
Elastic bands offer scalable resistance for shoulder, elbow, and wrist exercises. They support both stretching and strengthening, which is essential for reactivating neural pathways. Patients can perform abduction, extension, and flexion movements with minimal risk of strain. - Motor-Assisted Arm Trainers
These devices are designed for individuals with very limited voluntary movement. They use motors to guide the patient’s arm through a pre-set range of motion, promoting muscle memory and sensory feedback, which are critical for neuroplasticity. - Shoulder Pulleys
A simple but highly effective tool, shoulder pulleys hang from a doorway and allow patients to perform gentle, repetitive overhead movements. This helps reduce joint stiffness and can be used early in the recovery phase. - Hand Therapy Balls and Putty
These tools target the smaller muscles in the hands and fingers. By squeezing and manipulating different resistance levels, patients improve grip strength, coordination, and fine motor skills necessary for daily tasks like buttoning clothes or using utensils. - Forearm and Wrist Weights
Lightweight wrist cuffs or dumbbells help in muscle reconditioning. They can be used during seated exercises or combined with functional activities such as reaching or lifting small objects. - Mirror Therapy Boxes
A visual feedback method where the unaffected arm is reflected in a mirror, tricking the brain into believing the impaired limb is moving. This can stimulate motor cortex activity and encourage movement in the affected arm. - Robotic Arm Exoskeletons
These high-tech devices support complex, repetitive upper limb movements with precision. Used in clinics, they guide patients through customizable therapy plans, collecting data for progress tracking.
What lower limb strengthening machines support stroke recovery?
After a stroke, lower body rehabilitation focuses on strengthening the legs, improving joint mobility, and retraining the brain to walk again. Proper machines ensure both safety and progress.
- Recumbent Steppers (e.g., NuStep)
These machines allow patients to perform a stepping motion while seated, engaging the hips, knees, and ankles. They provide stability, reduce fall risk, and promote equal muscle activation in both legs. - Leg Press Machines with Adjustable Resistance
Leg presses help in building strength in the glutes, quadriceps, and hamstrings. Machines designed for rehabilitation have low starting resistance and can be adjusted incrementally as the patient gains strength. - Ankle Dorsiflexion Trainers
Stroke survivors often experience “foot drop,” a condition where the front part of the foot doesn’t lift properly. These trainers target the tibialis anterior muscle, helping to lift the foot during walking. - Seated Leg Curl and Extension Machines
These machines isolate specific muscles like the hamstrings and quadriceps, allowing patients to perform controlled movements without putting weight on their joints. This is critical for those who are early in recovery. - Resistance Bands for Lower Limbs
With varying tension levels, resistance bands can be looped around the thighs, ankles, or feet to support squats, leg lifts, and other targeted movements. They are especially useful for home rehabilitation. - Mini Steppers and Pedal Exercisers
These compact tools offer a stair-stepping or pedaling action while seated. They support coordination and rhythm, essential elements for rebuilding a natural walking gait. - Functional Electrical Stimulation (FES) for Legs
FES can be combined with these machines to activate specific leg muscles during the movement, further enhancing strength and improving neural connection.
What balance training equipment improves stability after a stroke?
Balance issues are common after a stroke due to muscle weakness, sensory loss, and impaired coordination. Training tools must be safe yet challenging to rebuild proprioception and core strength.
- BOSU Balls and Wobble Boards
These semi-stable platforms require constant micro-adjustments from the user, training the ankles, knees, and core. They’re excellent for dynamic balance and reflex development. - Balance Pads and Foam Blocks
Softer than wobble boards, these provide an unstable surface while standing. Patients can perform squats, single-leg stands, or weight shifts to re-engage stabilizing muscles. - Balance Rails and Bars
Parallel bars or wall-mounted handrails provide security during exercises. They help patients practice movements like side-stepping or shifting weight without fear of falling. - Tilt Boards and Rocker Platforms
These devices tilt in one or more directions and are ideal for ankle stability and postural control. They also retrain vestibular balance systems, which can be impaired after a stroke. - Stability Trainers with Real-Time Feedback
Digital systems that measure center of gravity and sway can guide users to correct their posture while providing visual cues. They enhance motor learning and encourage patient motivation through gamified training. - Step Platforms with Handrails
Step-up exercises train the hips and knees, encouraging symmetry and strength. With handrails, patients can focus on form and safety. - Laser-Cued Balance Beams
These use projected lines to guide foot placement during balance walking exercises. They improve spatial awareness and reduce reliance on external support.
What functional electrical stimulation (FES) devices assist in stroke rehabilitation?
FES devices electrically stimulate nerves and muscles that the brain can’t fully activate. This is particularly useful when voluntary movement is limited but nerve pathways are still partially intact.
- Foot Drop Stimulators
These devices attach to the lower leg and stimulate the peroneal nerve to lift the foot during the walking cycle. This aids in proper toe clearance and prevents tripping. - Hand FES Units
These portable units are often glove-based and stimulate the muscles of the wrist, hand, and fingers. Patients can practice gripping, releasing, and other fine motor skills critical for independence. - Multi-Channel FES Systems
These are programmable systems that stimulate several muscle groups at once, allowing for coordinated movement patterns in both upper and lower limbs. - FES-Assisted Cycle Trainers
Combining FES with a cycling motion helps activate muscles in sequence, promoting both aerobic endurance and motor retraining. These machines are used in clinics and advanced home rehab programs. - Wearable Neuroprosthetics
These sophisticated FES systems use motion sensors to trigger stimulation at the right time in a movement sequence. They are ideal for ambulatory stroke survivors looking to improve walking efficiency. - Clinically Guided FES Therapy Stations
In a supervised setting, these allow therapists to adjust intensity, frequency, and stimulation patterns based on real-time muscle response and rehabilitation goals.
What seated recumbent cardio machines are safe for stroke patients?
Stroke rehabilitation should include cardiovascular exercise to improve endurance and reduce the risk of future strokes. Seated machines reduce the risk of falls while allowing controlled movement.
- Recumbent Cross Trainers (e.g., NuStep)
These full-body machines combine leg and arm motion with a seated position, allowing patients to engage major muscle groups while staying supported. They’re ideal for improving stamina without taxing balance. - Motorized Passive/Active Pedal Trainers
These allow the patient to begin with passive movement and gradually shift to active pedaling as strength returns. They prevent joint stiffness and support circulation even in the early stages of rehab. - Arm-Leg Ergometer Machines
Users can pedal with their arms and legs simultaneously, boosting cardiovascular function and engaging bilateral movement, which is essential for neurological recovery. - Recumbent Bikes with Foot Support Straps
These bikes provide secure seating and hold the feet in place to prevent slipping. They help train the legs in a safe, rhythmic motion that mirrors walking. - Elliptical Trainers with Adjustable Seats
For patients transitioning from full support to partial standing, seated elliptical trainers provide a hybrid movement pattern that builds muscle coordination and endurance.
What hand and finger dexterity trainers help restore fine motor skills post-stroke?
Regaining control of the hands and fingers is essential for tasks such as eating, dressing, writing, and hygiene. Fine motor rehabilitation tools help recondition small muscle groups and improve neural precision.
- Therapy Putty
Therapy putty comes in different resistance levels, allowing patients to practice squeezing, pinching, and rolling. These movements strengthen finger flexors and extensors while improving grip coordination. - Finger Extension Bands
These bands are looped over the fingers to provide resistance when opening the hand. They’re crucial for combating spasticity and encouraging extension, which is often weaker than flexion post-stroke. - Hand Grip Strengtheners
Grip trainers include spring-loaded devices or foam-based grips. They target the intrinsic hand muscles and forearm, improving grip endurance needed for daily tasks like holding utensils or lifting objects. - Peg Boards and Dexterity Boards
These tools involve placing small pegs into holes or arranging objects using pincer grasp. They promote finger precision and bilateral coordination, and are used to retrain purposeful hand movement. - TheraBand FlexBars and Twist Trainers
These tools allow patients to practice controlled torsional movements of the wrists and forearms. They’re especially helpful for improving supination and pronation, which are essential for hand positioning. - Robotic Hand Therapy Devices
Some gloves and hand-based machines assist with passive and active-assisted movement. These tools guide the hand through repetitive actions to reinforce motor pathways and provide biofeedback. - Tactile Sensory Stimulation Tools
Tools with textured surfaces like spiky balls or textured grips help retrain sensory feedback. They are useful for improving sensation and tactile discrimination in the hand and fingers.
What bodyweight-supported treadmill systems help retrain walking after a stroke?
Bodyweight-supported treadmill systems (BWSTTs) help stroke survivors safely relearn walking by reducing the load on their lower limbs and preventing falls. They create a controlled, supportive environment for gait training.
- Overhead Harness Treadmill Systems
These systems use a harness to partially suspend the user above a treadmill. This unloads body weight, enabling earlier walking practice, even in patients with significant weakness or fear of falling. - Adjustable Support Percentage
The ability to gradually reduce support as strength and balance improve allows for progressive therapy. Clinicians can fine-tune the weight load from 100% support to 0%, tailoring the challenge level. - Split-Belt Treadmills
These treadmills have two independent belts, allowing each leg to move at a different speed. This helps correct gait asymmetries commonly seen after a stroke, such as one-sided dragging or shortening of step length. - Real-Time Biofeedback Integration
Some BWSTTs include sensors that provide visual and auditory feedback on stride length, foot placement, and weight distribution. This helps patients self-correct and enhances motor learning. - Therapist-Guided Gait Correction
Therapists can stand alongside the treadmill, providing manual assistance or adjustments. This close involvement allows for fine-tuning of posture, knee drive, and foot clearance. - Handrail and Handle Support Options
Systems often include side rails or forward handles that provide stability for patients who are gradually building independence and confidence while walking. - FES-Integrated BWSTT Systems
Advanced systems combine treadmill walking with functional electrical stimulation of leg muscles, reinforcing correct patterns of muscle activation and improving walking outcomes.
What smart rehabilitation robotics are used in stroke therapy?
Smart rehabilitation robotics support precise, repetitive movements which are critical for brain reorganization after a stroke. These devices enhance therapy intensity and track recovery metrics in real time.
- Robotic Arm Exoskeletons
These wearable devices assist with controlled, multi-joint upper limb movements. Patients can perform reaching, lifting, and grasping tasks with adjustable resistance and support levels. - End-Effector Robotic Devices
Instead of being worn, these robotic arms hold and move the patient’s hand or foot in a predefined path. They’re ideal for replicating natural movement patterns repeatedly and accurately. - Bilateral Arm Trainer Robots
These systems coordinate movements of both arms simultaneously. The non-affected arm assists the affected one, improving neural synchronization and reducing compensation habits. - Lower Limb Robotic Gait Trainers
Devices like Lokomat guide leg movements while the user walks on a treadmill. They ensure accurate hip and knee flexion angles, and assist in retraining normal stride rhythm. - Adaptive Resistance and Support
Smart robots adjust their level of assistance based on real-time performance. As patients improve, the system offers less support, encouraging more active participation. - Progress Tracking Dashboards
Many robotic systems provide immediate feedback and long-term data tracking. Therapists and patients can monitor joint angles, repetition counts, force output, and range of motion gains. - Virtual Reality Integration
Some robotic rehab tools include gamified environments that increase engagement. Patients may complete tasks within a VR setting that mirrors real-life scenarios, helping transfer gains to daily activities.
What resistance bands and pulley systems are best for home-based stroke rehab?
For patients continuing therapy at home, resistance bands and pulley systems are essential. They’re cost-effective, portable, and versatile, allowing for strength and flexibility exercises without complex machines.
- Door-Mounted Shoulder Pulleys
These pulleys allow patients to perform active-assisted shoulder flexion and abduction exercises. They’re ideal for those recovering shoulder range post-stroke and can be used while seated or standing. - Color-Coded Resistance Bands
Bands come in a range of resistance levels, from very light (yellow) to extra heavy (black). This allows patients to gradually progress in strength and customize difficulty based on limb function. - Loop Bands for Legs and Hips
Loop-style resistance bands are used for lateral steps, seated knee extensions, and leg lifts. They help strengthen the glutes, thighs, and hip abductors—all critical for standing and walking. - Figure-8 Bands and Handles
These provide a secure grip for individuals with limited hand function. They can be used for bicep curls, shoulder presses, and trunk rotations with better hand control. - Anchor Systems for Custom Setups
Resistance bands can be anchored to furniture or specialized mounts, allowing exercises from various angles to target multiple joints and muscles. - Pulley Towers with Weight Adjustments
Some at-home pulley systems have weighted stacks or resistance mechanisms, offering more precise and adjustable therapy options than simple elastic bands. - Elastic Tubes with Handles
These are especially helpful for stroke survivors with reduced grip strength. Padded handles or wrist cuffs allow for easier control and safer performance.
What parallel bars and gait training frames assist in walking reeducation?
Walking recovery often starts with supported environments where the risk of falls is minimized. Parallel bars and gait frames provide the necessary structure to rebuild walking mechanics step by step.
- Adjustable Parallel Bars
These allow for customized height and width, supporting users of different sizes and progress levels. Early-stage patients can practice standing, weight shifts, and side-stepping with full support. - Gait Training Frames with Wheels
These devices offer both support and mobility. Some models include braking systems or forearm supports to help with forward movement and upright posture. - Overhead Suspension Integration
Parallel bars with a suspension harness help prevent falls and provide partial bodyweight support. This feature encourages more confident gait practice in weak or high-risk patients. - Markers and Floor Guides
Visual aids on the floor help patients align their steps, improve foot placement, and train for stride symmetry. They provide external feedback that promotes correct repetition. - Incline Parallel Bars
Some rehab settings use slightly inclined bars to challenge leg muscles and train uphill walking mechanics in a controlled way. - Multifunction Frames
These are adjustable systems that can convert between parallel bar configurations and walking frames. They provide flexibility for clinics or home rehab environments with limited space.
What cognitive-motor training equipment offers visual feedback for stroke recovery?
Cognitive-motor training tools are designed to stimulate both brain and body during rehabilitation. These tools promote coordination, attention, and memory, which are often affected post-stroke. Visual feedback enhances neuroplasticity by helping patients correct movement errors in real time.
- Reaction Light Boards
These interactive boards light up randomly and require patients to touch the lights quickly. This sharpens reaction time, improves visual scanning, and boosts upper limb speed and accuracy. - Virtual Reality (VR) Therapy Systems
VR rehab systems immerse patients in interactive environments that challenge both physical movement and cognitive tasks. Patients might walk through virtual mazes or reach for moving objects, which trains balance, coordination, and decision-making. - Balance Boards with Visual Targets
Devices like digital force platforms track how a patient distributes weight while standing or shifting. The screen shows real-time movement, enabling users to adjust their center of gravity and posture. - Interactive Step Systems
These platforms light up or produce audio cues to prompt stepping in specific directions. Patients must quickly identify and respond to cues, improving dynamic balance and cognitive responsiveness. - Touchscreen Puzzle Trainers
Systems with memory, sequencing, or matching games require both hand interaction and mental focus. These tools support problem-solving, bilateral hand use, and fine motor control. - Biofeedback Monitors
Wearable sensors display metrics like heart rate, muscle activity, or step count. Patients become more aware of their exertion and progress, which builds motivation and reinforces task accuracy.
What stationary pedal exercisers support passive and active motion during rehab?
Stationary pedal exercisers are a versatile solution for restoring joint movement, circulation, and endurance in patients who may not yet be ready for full weight-bearing exercise. They support both upper and lower limb rehab.
- Seated Leg Pedal Exercisers
These devices allow patients to perform cycling motions while seated in a chair or wheelchair. They encourage blood flow, reduce joint stiffness, and enhance coordination between the knees and hips. - Motor-Assisted Pedal Trainers
For users with very limited mobility, these trainers use built-in motors to guide the limbs through a natural pedaling motion. They help maintain muscle activity and range of motion passively. - Dual-Use Arm and Leg Pedal Machines
These compact devices can be placed on the floor for legs or on a table for arms. This dual function allows stroke survivors to engage in full-body conditioning even with mobility restrictions. - Models with Adjustable Resistance
Resistance settings help transition users from passive to active engagement. As strength and confidence grow, resistance can be gradually increased to improve muscle conditioning. - Reverse Pedaling Function
Reverse cycling activates different muscle groups and enhances neuromuscular control. It’s especially helpful for retraining coordination and supporting motor learning. - Digital Display Models with Progress Tracking
Some models feature LCD screens that display distance, time, RPM, and calories burned. This provides measurable benchmarks that can motivate users and inform therapists. - Pedal Straps for Safety and Alignment
Pedal exercisers often include foot straps to secure the limbs and prevent slipping, ensuring a safer experience for users with limited foot control or spasticity.
What wheelchair-compatible gym equipment is best for stroke survivors?
Inclusive gym equipment ensures that wheelchair users can engage in safe and effective workouts. These machines allow for cardiovascular and strength training without the need for standing or transferring.
- Resistance Machines with Swing-Away Seats
These allow users to roll directly into position without leaving their wheelchair. They enable upper and lower body resistance training and are fully adjustable for height and reach. - Seated Upper Body Ergometers (Arm Bikes)
These are ideal for cardiovascular conditioning. They improve heart health, shoulder mobility, and endurance while being fully accessible from a seated position. - Cable Pulley Systems with Extended Handles
These systems are adjustable in height and feature long handle attachments that allow for rows, presses, and other movements with limited arm mobility. - Weighted Wrist and Ankle Cuffs
These are perfect for adding resistance to controlled movements such as arm lifts or leg extensions, without the need for gripping dumbbells or holding equipment. - Wall-Mounted Resistance Bands
These bands offer scalable resistance and are positioned to be easily used from a seated position, facilitating strength exercises for both upper and lower body. - Pedal Exercisers with Hand Cranks
These compact machines allow arm cycling at adjustable heights and resistance levels. They’re ideal for improving range of motion and cardiovascular health in wheelchair users.
What isometric exercise tools are suitable for stroke patients with low mobility?
Isometric tools allow patients to activate and strengthen muscles without moving their joints. This is beneficial for those with spasticity, limited range of motion, or fatigue.
- Squeeze Balls and Therapy Grips
These promote hand and forearm strength through static pressure. By squeezing and holding, users improve grip endurance and muscle activation without requiring joint movement. - Isometric Leg Press Devices
Seated leg press tools allow users to push against a fixed resistance point. This helps maintain muscle strength in the quadriceps and glutes, especially when dynamic exercises are not yet possible. - Wall Pushes and Static Arm Holds
Pushing against a wall or holding arms out in place activates shoulder, chest, and back muscles. These exercises are safe and require no equipment but can be enhanced with light resistance. - Resistance Bands Anchored for Static Pulls
Patients can hold a band in a fixed stretch, engaging target muscles. This approach builds endurance and neural engagement even when full movement is not achievable. - Grip Dynamometers
These tools not only help build grip strength through static effort but also provide numerical data on force output, which is valuable for tracking rehabilitation progress. - Compression Therapy Tools
These devices stimulate blood flow and maintain muscle tone through gentle squeezing cycles, particularly in the legs. They are passive but support tissue health in low-mobility users.
What multi-functional rehab stations are used in clinical stroke therapy programs?
Multi-functional rehab stations combine several therapies into one modular unit. These stations are commonly found in outpatient clinics and neurological rehab centers to streamline treatment.
- Full-Body Cable Systems
These machines include adjustable pulleys, bars, and resistance options that target both upper and lower limbs. They allow for seated or standing use and support diverse therapeutic goals. - Touchscreen-Guided Therapy Stations
These provide step-by-step instructions and progress tracking, guiding patients through custom routines while adjusting difficulty based on user performance. - Combination Arm-Leg Trainers
These hybrid units synchronize limb movement, which reinforces coordination between left and right sides—a critical focus in stroke rehabilitation. - Motorized Resistance Trainers
These offer isotonic and isometric resistance modes that adapt in real time. They are useful for gradual strength progression in weakened limbs. - Cognitive-Motor Integration Modules
Some stations include puzzle solving, sequencing games, or memory tasks paired with physical movements. This enhances the brain’s ability to connect mental tasks with motor responses. - Multi-Angle Weight Benches with Support Harnesses
These enable safe positioning for various exercises and can be used in both seated and reclined positions to accommodate different physical capabilities. - Data-Driven Feedback Systems
Built-in software collects performance metrics like time, repetition count, and force output. This allows therapists to monitor trends and adjust treatment plans effectively.
Conclusion
Stroke rehabilitation demands a structured, multi-phase approach — one that combines safety, progression, and neuroplastic engagement. The right equipment bridges the gap between clinical care and functional independence. Whether you’re seeking seated cardio machines, hand therapy tools, gait trainers, or high-tech robotics, every device plays a vital role in recovery.
At Max Gym Gear, we provide medical-grade, stroke-friendly gym equipment tailored for home users, clinics, and rehab centers. We offer discreet overnight delivery, financing options, and a 30-day replacement or full refund policy. All products come with a 1-year warranty and are shipped with full privacy and tracking assurance.
Want to buy gym equipment online? Fill out our contact form — we ship within 24–48 hours in the USA and Canada, and deliver internationally in 5–7 days. At Max Gym Gear, your recovery journey is our mission.